If the argument that buildings can shape happiness is true, it-s time we reimagine our hospitals for a post-COVID world where the refuge for the sick don-t turn into infection hot zones

Unlike modern hospitals, the Bai Jerbai Wadia Hospital for Children in Parel is a colonial structure that follows some of the structural principles of natural lighting, low windows, wide vestibules and greenery that architects are advocating. Pic/ Suresh
In a March 2020 article for the Washington Post, Emily Anthes, author of the recently published title, The Great Indoors: The Surprising Science of How Buildings Shape Our Behavior, Health, and Happiness, writes while discussing a SARS outbreak, "One irony of an infectious-disease outbreak is that it turns hospitals, which should be a refuge for the sick, into hot zones, putting everyone inside at risk." In the next paragraph, she adds, "When doctors in Wuhan, China, where the new virus first emerged, studied 138 early cases, they concluded that 41 per cent of patients had most likely contracted the disease in the hospital."
ADVERTISEMENT

People line up at Nair Hospital for COVID-19 tests. In an ideal healthcare situation, say experts, tests should be conducted outside hospitals with only those advised by their GP, heading to the hospital for further consultations. This would decentralise hospitals and prevent over crowding
She lists some simple modifications, including where hand sanitisers are kept—closer to the care area instead of at doors and entrances—and humidifying the air. Other plans involve greater modifications and rethinking, even, how hospitals ought to function in the first place.
 Manoj Choudhury
Manoj Choudhury
Manoj Choudhury is director at Edifice Consultants, an architectural firm which has experience in setting up hospitals such as the Tata Memorial Hospital-s Cancer Centre along with Tata Trusts at Varanasi, is currently working on the Cancer Grid Programe with Tata Trust for setting up multiple cancer centres across the country, the revamp plan for Bai Jerbai Wadia Hospital for Children at Parel, extension of Breach Candy Hospital and COVID-19 centres across Maharashtra and Uttar Pradesh along with Tata Trust. He says that many regulations for ensuring infection control and social distancing, are already in place in guidelines provided by the National Accreditation Board for Hospitals. For instance, corridors and passageways in hospitals ought to have a minimum width of 2.4 metres. And, in an OPD, any doctor should have at least six waiting chairs for patients.
Tiny modifications can also be brought in to ensure that patients and outsiders don-t cross paths. For starters, says Rahul Kadri, partner and principal architect of IM Kadri Architects, simply demarcating different lift banks and segregating pathways within an existing structure can ensure that those who are infected or ill do not come in contact with those who possibly aren-t. Another important aspect of reducing the spread of infection within the hospital structure is the air-conditioning system and the over-reliance of modern buildings on the same. The current systems, he says, circulate 90 per cent of the same air, bringing in only five per cent of fresh air in ward rooms.
 Rahul Kadri
Rahul Kadri
"If we optimise this, 90 per cent can be reduced to 80 per cent, which is still a high figure," he says, even adding better filtration systems is risky, adding that instead, here on, new construction of hospitals could look at biophilic designs—a design theory that seeks to connect building occupants more closely to nature by incorporating natural ventilation, minimise heat gain, daylighting, natural landscape features for creating a more productive and healthy built environment for better recovery.
Evidence supports the idea. A 1984 study by Roger Ulrich, professor of architecture at Texas A&M University and a faculty fellow of the Center for Health Systems and Design, found that post-operative patients, who had a view of nature from their windows recovered faster than those whose windows overlooked brick walls.

Dr Benny Kuriakose
Dr Benny Kuriakose, conservation architect from Chennai, known for designing structures built from natural materials, says that essentially, hospitals shouldn-t look like hospitals. "Often people who work in the IT industry step out of office at 5.30 pm to head home and realise that it had rained in the day and they were unaware. Imagine that those who work in hospitals are often there for more than half the day. Many hospitals also don-t provide for natural lighting. They need to. Hospitals need to give a more comfortable feeling to patients and those who work there. Patients should have low windows next to them and there should be more greenery. We should have courtyards to give natural light and fresh air."
Kadri makes another point. Isolating one part of the hospital from another to curtail the spread of infection. Instead of building structures as one unit, keeping two or three separate wings, connecting them only with one corridor will allow for greater isolation of diseases within a hospital. A challenge everyone is facing in the current scenario. It will also, for instance, help patients in urgent requirement of dialysis, access healthcare without having to enter a structure where a deadly virus lurks.

Dr Vandana Rajesh
Marol-s Seven Hills Hospital offers an example of isolation to protect healthcare workers. Dr Vandana Rajesh, a consultant intensivist at the COVID-19 Hospital, says the ICU beds here are each contained within a glass door cubicle as large as 10x10 feet. Some have negative pressure, which means that aerosols that are thrown out of the cubicle are filtered before they go out of the cubicle. Those outside the cubicle, including health workers, are exposed to aerosols with lesser concentration of the virus. "Once you already have a viral load, a six-feet distance between two infected patients doesn-t matter. But, it-s important for the health worker not to be infected," she adds. In May, it had been reported that over 70 junior doctors from across the city-s medical colleges had tested COVID-19 positive. The ICU cubicles were an existing feature in the hospital, something that most other hospitals in Mumbai don-t have.
Another way of preventing crowding inside the hospital is to screen who enters.
Choudhury points out that in the pre-COVID world, we could enter any hospital, whatever our needs. The out-patient department would be on the ground floor, typically, but in some cases even in higher floors. However, in some projects the OPD is set up outside the hospital area with a registration desk that is supported by a telemedicine infrastructure. Manned by junior doctors, who will check patient records and symptoms, only those who need to be admitted or see a specialist will be allowed in. It-ll be the same for those who contact their local general physician and come with a prescription for either further tests or consults. "This is what is done in the UK and US where people go to hospitals only at the recommendation of their GP. No one walks into a hospital, directly and unguided." In Dharavi, he adds, local clinics and doctors were leveraged to control the COVID-19 pandemic.

Rajeev Sadanan
But, this will be possible, points out Rajeev Sadanan, CEO of Health Systems Transformation Platform, and Former Additional Chief Secretary Health for Kerala, only if the primary care system inspires confidence.
"People are worried that they won-t get quality care outside of the big hospitals. But the primary care provider, if relied upon, can assess risk factors and tell a patient if they are having a heart attack or a gastric attack and, accordingly direct them to appropriate treatment," he says, adding that ideally the healthcare system should be like a pyramid with the maximum number of people seeking treatment at the lowest level and the smallest amount being treated at expensive, super speciality, centres. However, what-s unfolding in India is the opposite, an inversion of the pyramid. To resolve this, ideally, the government should step in to organise health care with primary care as the foundation with referral pathways to higher levels of care.
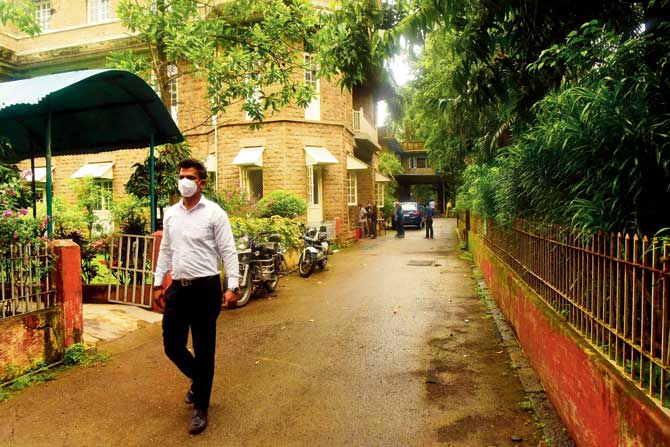
Minnie Bodhanwala, CEO of Wadia Hospital, says the heritage structure allows for its young patients to connect with nature. Its windows allow for natural lighting and better ventilation. Many wards have balconies attached and there-s a play area where children can even cycle, under supervision. Pic/Suresh Karkera
But, none of these will work, points out Choudhury, unless we look beyond doctors when speaking of health workers and also include the skilling of nurses and paramedics, and think about the infrastructure for them, including living quarters. "For instance, you want a junior doctor at a South Bombay hospital, but their salaries are so low that they can-t afford the rent to live and work there. City doctors don-t want to move to smaller towns, so setting up an AIIMS in Gorakhpur won-t help decentralise the Delhi centre, because there are not enough doctors, nurses or paramedics there."
Catch up on all the latest Mumbai news, crime news, current affairs, and a complete guide from food to things to do and events across Mumbai. Also download the new mid-day Android and iOS apps to get latest updates.
Mid-Day is now on Telegram. Click here to join our channel @middayinfomedialtd and stay updated with the latest news
 Subscribe today by clicking the link and stay updated with the latest news!" Click here!
Subscribe today by clicking the link and stay updated with the latest news!" Click here!






